Oxygen crisis and the fault in our healthcare system sdf
 Farida Akhter || Friday 09 July 2021 ||
Farida Akhter || Friday 09 July 2021 ||
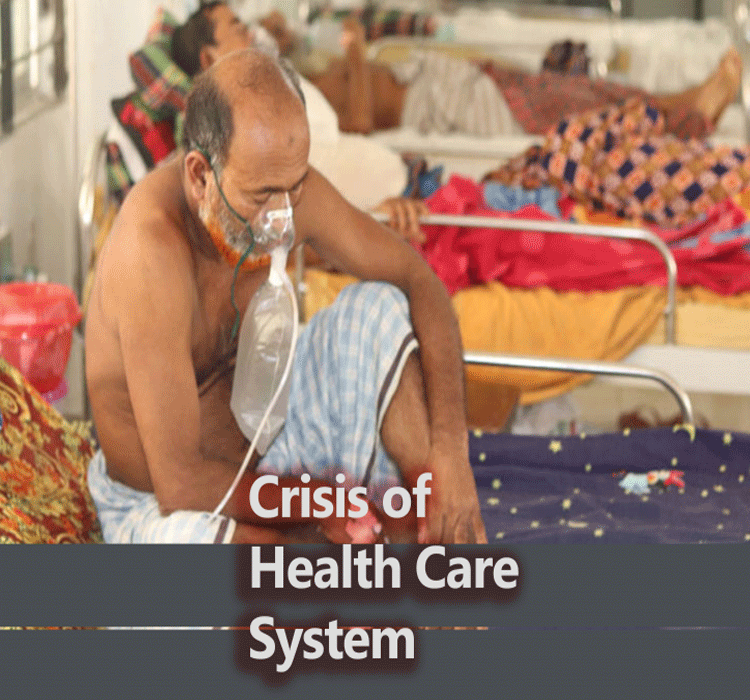
A lack of oxygen support systems in Bangladesh’s public healthcare system are a serious detriment in the battle against Covid-19
The government did not use the time they had over one year to enhance the facilities at the district hospitals with equipment and human resources.
Deaths from Covid infections are rising at an alarming rate in district hospitals. During the first week of July, the deaths per day rose to record levels in Bangladesh since the Covid pandemic began. On 5 July,164 deaths were recorded, the highest number yet. We can only hope it does not increase further.
In 2020, the death toll was the highest in the Dhaka division, particularly in the metropolitan Dhaka city. But with the rise of infections in the surrounding districts, the death figures are higher in the divisional hospitals. On 5 July, 55 deaths were recorded in Khulna, followed by 40 in Dhaka, 18 in Chattagram, 16 each in Rangpur and Rajshahi, and the rest 19 in other districts. Over 75% of Covid deaths in 24 hours are recorded in hospitals outside Dhaka. This is indeed alarming and also gives a tragic picture of the precarious situation of our health sector.
Perhaps many of these deaths could have been prevented. Last week, several reports were published by electronic media outlets as well as by print media outlets about the crisis of high-flow oxygen support in hospitals in the Khulna and Rajshahi divisions.
At the Satkhira Medical College Hospital, five Covid patients died following a disruption in oxygen supply. In this hospital, more than 100 patients were admitted; however, they have only 12 high-flow nasal cannulas (HFNC) at the hospital. In Bogura, at least 13 patients died in two hospitals in the 24 hours of July 2 because of the shortage of high-flow oxygen support provided through HFNCs.
One of these hospitals has only two HFNC devices. Four patients died in Pabna hospital due to the oxygen supply problems. The hospital was seeing a crisis of oxygen as the number of Covid patients increased. Many patients had to arrange oxygen cylinders personally as of 5 July. A similar situation exists in the majority of district and divisional level Medical College hospitals. The hospitals in Dhaka are now full of patients from other districts.
According to the World Health Organization (WHO), ICU and ventilator support is needed by 20% of Covid-19 infected patients; among them 15% who present strong symptoms and 5% who find themselves in a critical condition. Additionally, older patients with other chronic diseases or comorbidities require ICU support.
Most of the Covid-positive patients are not advised to be admitted to the hospitals. They can be treated at home by staying in isolation and with the medical advice of doctors. Critical Covid patients are hospitalised mostly when they require oxygen or have respiratory complications. Oxygen supply in the hospitals is also required by non-Covid critical patients suffering from non-communicable diseases.
According to the Directorate General of Health Services (DGHS), the oxygen supply at government hospitals doubled amid the rise in Covid patients to around 200 tonnes a day. The amount of oxygen necessary for Covid patients has doubled the requirement of oxygen in hospitals. There are a total of 13,984 isolation beds at dedicated Covid-19 hospitals across the country – of which 399 are ICU beds. Many Covid -19 patients are suffering from a lack of oxygen support and many are dying.
This did not come as a surprise to many people. Our healthcare system is skewed towards providing the best service to urban-dwellers, particularly to the elites: the rich, the government officials, politicians, businessmen, etc. The primary healthcare goes down to the rural level; the secondary and the tertiary level health facilities are located in the cities, more particularly in Dhaka, the capital city.
Most of the government hospitals all over the country are equipped with the necessary ICU facilities . Yet many patients have to travel to Dhaka in the government and private hospitals for superior treatment of non-communicable diseases. The lack of manpower for managing the ICUs is also an important factor for the lack of services.
In the public healthcare system, from community clinics, Upazila Health Centres to district hospitals, the working class get outdoor treatment and get free medicine for common ailments. Few are advised for further tests to diagnose the diseases. Acute respiratory infections, which may require the support of oxygen, are referred to the district hospitals or hospitals in Dhaka.
Published: The business standard; 08 July, 2021
Every day, hundreds of patients fall into critical conditions, and seek healthcare at tertiary level hospitals such as Dhaka Medical College Hospital, Bangabandhu Sheikh Mujib Medical University, Suhrawardy Hospitals, etc. They need cardiac care, services offered in intensive units, oxygen, and ventilator supports.
After the outbreak of the Covid-19 pandemic, due to a lack of preparation, the initial response of the government and private hospitals was not to take any patients. The hospitals were running empty for months until the government made a decision regarding Covid dedicated beds in the hospitals. The denial of health services both by the public and private hospitals raised major ethical and human rights concerns.
The privatization of healthcare, following the neo-liberal policies, resulted in the public healthcare system providing only 30% of services. The Covid-19 pandemic shows the need to have strong public health services which cannot be achieved by the private sector alone. The out-of-pocket expenditure of patients has increased from 67% in 2012 to 73% in 2017 in public hospitals according to the World Bank. This is an index of increasing dysfunctionality of public health, particularly when public hospitals are the only sources for the working class to receive healthcare.
The private profit-oriented hospitals and clinics, allowed to provide Covid-19 care, have been using the opportunity of providing Covid-19 treatment merely as a commercial venture. To them, health services are market commodities and the pandemic is an opportunity to maximize profits, taking advantage of the fear of the people of the potential fatality of a Covid-19 infection. However, commercial Covid care did not prove to be any better than the public health services.
Unfortunately, the government did not use the time they had over one year to enhance the facilities at the district hospitals with equipment and human resources. It is disheartening to know that there are no ICU facilities at 37 out of 64 districts in the country according to the DGHS. A total of 2,420 ICU beds are available in the country with 1,218 (50%) of them at Dhaka Metropolitan and 59 (2%) at Chattogram Metropolitan. The rest (1143) are available in 25 districts.
Covid patients with an oxygen saturation below 90 need to be admitted to ICU with high-flow oxygen support. The government considers hospital beds with HFNC facilities as equivalent to ICU beds. As many as 11 districts do not have nasal cannula facilities.
This shortage should not come as a surprise to the government. The government already approved projects to set up ICU units in all district hospitals at the ECNEC meeting on 2 June, 2020. This also included training 3,500 health workers and the purchase of equipment to set up PCR labs and ICUs. This has not been implemented yet.
We cannot deal with this grave crisis with a weak public health infrastructure and the policy of privatizing medical care. While we must shift away from the neoliberal policies that have been dismantling our public healthcare system, we must also find innovative ways of striking a balance between public responsibility and the accountability of private sectors.
We need to develop a robust public health care system by not undermining the positive role the private sector may play. Market and private investment, if geared with responsibility and accountability, may impart dynamism both into the economy and the sense of responsibility within the government. That could save the lives of our people.
Lockdown is only one of the few measures against community transmission, but for those who are already infected and need hospital care, the facilities need to be better equipped in order for patients not to succumb to a lack of oxygen.